Addressing Health Disparities in the Undergraduate Curriculum: An Approach to Develop a Knowledgeable Biomedical Workforce
Abstract
Disparities in health and healthcare are a major concern in the United States and worldwide. Approaches to alleviate these disparities must be multifaceted and should include initiatives that touch upon the diverse areas that influence the healthcare system. Developing a strong biomedical workforce with an awareness of the issues concerning health disparities is crucial for addressing this issue. Establishing undergraduate health disparities courses that are accessible to undergraduate students in the life sciences is necessary to increase students’ understanding and awareness of these issues and motivate them to address these disparities during their careers. The majority of universities do not include courses related to health disparities in their curricula, and only a few universities manage them from their life sciences departments. The figures are especially low for minority-serving institutions, which serve students from communities disproportionally affected by health disparities. Universities should consider several possible approaches to infuse their undergraduate curricula with health disparities courses or activities. Eliminating health disparities will require efforts from diverse stakeholders. Undergraduate institutions can play an important role in developing an aware biomedical workforce and helping to close the gap in health outcomes.
INTRODUCTION
Disparities in health and healthcare between segments of the U.S. population have been well documented and are a major public health concern (Centers for Disease Control and Prevention [CDC], 2013). Health disparities are defined as differences in health outcomes between segments of the population and are usually a reflection of social inequalities (CDC, 2013). Differences in life expectancy, morbidity, disease risk factors, and quality of life are observed among segments of the population in association with factors such as socioeconomic status, race/ethnicity, and education level (CDC, 2013). For example, disparities in life expectancy exist within sectors of the population in the United States in relation to race, income, and geographic location (Murray et al., 2006). Notably, there have been consistent disparities in mortality between black and white Americans, who currently have a life expectancy of 74.3 and 78.4 yr, respectively (U.S. Census Bureau, 2012). Also, when considering a combination of sociodemographic characteristics and place of residence, data show life expectancy gaps of up to 15 yr among sectors of the population (Murray et al., 2006). The urgency to address health disparities is heightened by ongoing changes in U.S. demographics. Significantly, some populations that are most vulnerable to health disparities are among the fastest-growing segments within the United States (Freid et al., 2012). Also, the percentage of households earning less than twice the federal poverty level, which are considered to be low-income households, have increased in the past decade and account for more than 40% of the population (U.S. Census Bureau, 2012). Owing to these circumstances, significant value has been given to setting forth a national policy that addresses health disparities. This need is exemplified by the publication of Healthy People 2020, a continuous plan that sets the national agenda to improve the health of all Americans and that has as one of its overarching goals an emphasis on eliminating health disparities (U.S. Department of Health and Human Services, 2014).
Addressing health disparities will require a multipronged approach that involves a diverse set of stakeholders and targets key areas of the healthcare system. One critical area to target is the future scientific and medical workforce. Awareness of health disparities remains low among the general public and among racial minorities, who have low levels of appreciation of the disparities disproportionally affecting their own communities (Benz et al., 2011). It is imperative to train knowledgeable and passionate biomedical professionals from diverse backgrounds to have a solid understanding of health disparities (Lunn and Sanchez, 2011). Even though there have been efforts to train the current health workforce in the broad issues of health disparities and to create courses for the medical school context (Ross et al., 2010; Vela et al., 2010), there are advantages to starting these efforts earlier, at the undergraduate level. Exposing undergraduate students through courses and other activities to issues in health disparities is central to better preparation, engagement, and motivation of the future biomedical workforce. Owing to the complexity of the healthcare system, it is important to target students pursuing a variety of careers, including future physicians, health professionals, scientists, and researchers, thus helping to advance health equity from wide-ranging approaches.
Institutions should engage undergraduate students, especially those pursuing majors that might lead to biomedical careers, to have an increased appreciation of the impacts of health disparities. A greater inclusion of undergraduate health disparities courses at all higher education institutions, particularly at minority-serving institutions (MSIs), would make more students aware of the issues and may encourage them to engage in addressing them during their careers.
Current Landscape of Health Disparities Courses in U.S. Universities
To understand the level of inclusion of health disparities as a topic in institutions that grant undergraduate degrees, we conducted a review of the courses offered in the 2013–2014 academic year in a sample of institutions randomly selected from the Carnegie Classification of Institutions of Higher Education data set (Carnegie Foundation for the Advancement of Teaching, 2012). We limited our analysis to institutions with total student Fall enrollment counts of at least 2000 undergraduate and graduate students and, in order to focus on undergraduate health disparities education, to institutions that granted at least a bachelor's degree. The institutions were separated into three groups, including doctorate-granting universities (i.e., very-high-level research universities, high-level research universities, and doctoral universities), master's colleges and universities (i.e., master's colleges and universities with large, medium, and small programs); and baccalaureate colleges (i.e., baccalaureate colleges offering degrees in the arts and sciences and in diverse fields). In addition, a fourth, separate group comprising all historically black colleges and universities (HBCUs) and Hispanic-serving institutions (HSIs) with more than 2000 enrolled undergraduate and graduate students. Subsequently, each of these groups of institutions was ranked by student enrollment, and a random sample of institutions was designated by employing a random number generator to select row numbers. The selection included 43 doctoral universities (from a pool of 288 institutions, 15%); 31 master's universities (from a pool of 601 institutions, 5%); 14 baccalaureate colleges (from a pool of 188 institutions, 7%); and 12 MSIs (from a pool of 119 HBCUs and HSIs, 10%). The online university catalogues for the 2013–2014 academic year were used to search course titles and descriptions and find courses in any discipline with substantial content on health disparities. All undergraduate courses were taken into account, and no distinction was made for major, course level, or course type (i.e., elective or required). To be considered, a course had to have a focus on health or the healthcare system and include health disparities as part of the title or course description. For example, a public health course that is described as including a discussion of public health disparities, issues in public health, and global health issues would be classified as containing substantial health disparities content. The course prefixes were used to determine which departmental units aligned with a specific course.
Approximately 40% of the institutions analyzed offered a course in which topics on health disparities were a significant component of the course's content (Figure 1). This figure was greatly reduced for MSIs, which include such courses at a 25% rate. There could be various reasons why MSIs do not include such courses at the same level as institutions not classified as MSIs, including reduced resources to provide such courses. It is of particular importance to increase the inclusion of health disparities courses at these institutions and to consider strategies that are mindful of the MSI context and the possible challenges these institutions face. MSIs serve students from communities traditionally burdened by differential health outcomes, and these students play a critical role in increasing the diversity of the biomedical workforce and reducing health disparities (Beal, 2004; Grumbach and Mendoza, 2008). Offering a health disparities course at MSIs provides the distinct advantages of exposing minority students to these issues and encouraging them to pursue careers in health disparities. MSIs currently produce the largest number of underrepresented minority science, technology, engineering, and mathematics (STEM) graduates, including those continuing on to earn graduate degrees in STEM disciplines (Stage and Hubbard, 2009; Clewell et al., 2010; Whittaker and Montgomery, 2012). These minority students can play a significant role in reducing health disparities (Beal, 2004; Grumbach and Mendoza, 2008). For example, physicians from racial and ethnic minorities, who currently are severely underrepresented in health professions, are more likely to serve at-risk minority populations (Komaromy et al., 1996; Beal, 2004; Grumbach and Mendoza, 2008). Moreover, patients treated by physicians from similar cultural backgrounds report better healthcare outcomes (Beal, 2004). Because self-identity and the sense of responsibility to a particular community can be a powerful personal motivator (Ratanawongsa et al., 2006; Odom Walker et al., 2010), exposing minority STEM students to health disparities courses might encourage more of them to engage in addressing health disparities issues during their careers. Therefore, it is of particular importance to offer health disparities courses at MSIs, in order to provide minority students with information about health disparities, encourage them to pursue biomedical careers related to health disparities, and, thus, help increase their representation in these professions.
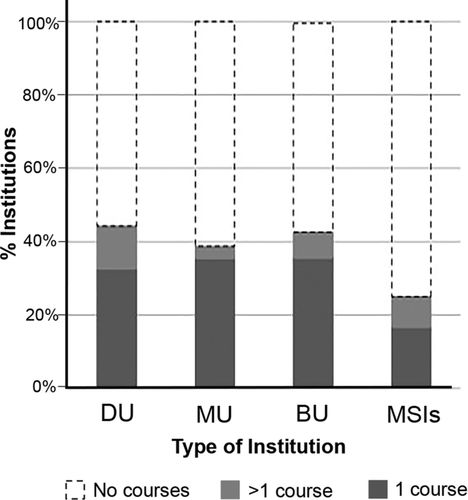
Figure 1. Percent of institutions that include one course, more than one course, or no courses addressing health disparities. Data are taken from a random sample of colleges and universities classified by the Carnegie Classification of Institutions of Higher Education. Only institutions with more than 2000 students were included in the analysis. Doctoral universities (DU) include 15% of all institutions that grant a doctoral degree (n = 43). Master's universities (MU) include 5% of all institutions that grant a master's degree (n = 31). Baccaleaureate universites (BU) include 7% of all institutions that only grant bachelor's degrees (n = 14). MSIs include 10% of all HBCUs and HSIs (n = 12). The online university catalogues for the 2013–2014 academic year were mined, and courses in any discipline with substantial content on health disparities were catalogued.
To increase the access to health disparities courses, it is necessary that students are aware of such courses during their educational trajectory. Particularly for institutions that offer a large variety of courses, it is possible that students will be more familiar with the courses that are offered by the department of their major or related disciplines. Of the institutions surveyed, 75% of the courses offered by these institutions were housed from departmental units in the social sciences (26%), public health (28%), and nursing (23%; Figure 2). However, students who will pursue careers in biomedical research and health professions are likely to be enrolled in undergraduate degrees in the life sciences. For example, medical school applicants are predominantly pursuing science undergraduate degrees (∼67%), including biology as their principal major (∼53%; Association of American Medical Colleges [AAMC], 2013). Even though 40% of all institutions surveyed in this study offered health disparities courses, it is possible that the visibility of these courses is limited for undergraduate students in biology majors, including those in the premedical track. It is particularly important to engage these students, possibly by including health disparities courses in the curriculum of biological sciences departments or other related disciplines. Alternatively, life sciences departments can increase the visibility of existing courses in other departments and encourage students to participate in them, when offered.
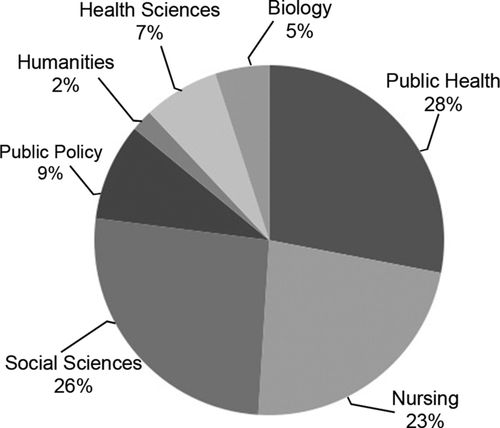
Figure 2. Percent of health disparities courses by discipline. Of the 88 university catalogues analyzed, a total of 43 courses were focused on health disparities. Approximately 75% of these courses were evenly distributed between departments in public health, social sciences, or nursing. Biological sciences departments only managed 5% of the courses related to health disparities. The remaining courses were catalogued as public policy (9%), health sciences (7%), and humanities (2%).
Approaches to Incorporate Health Disparities as a Topic in the Undergraduate Curriculum
Incorporating health disparities as a topic in undergraduate studies can be accomplished through diverse approaches. These efforts can include the addition of new courses to the curriculum, the development of interdepartmental collaborations that make existing courses more visible to science majors, or the formation of partnerships with diverse stakeholders.
Health disparities courses can be a valuable asset to the undergraduate life sciences experience, and developing them should be seriously considered. The current guidelines for undergraduate biology and premedical education, which include an interdisciplinary focus and the presence of both a scientific and social sciences foundation, can be effectively incorporated into a health disparities course (AAMC and the Howard Hughes Medical Institute, 2009; AAMC, 2011; National Research Council, 2009; Awosogba et al., 2013). For example, we recently developed a course on the biology of health disparities at the University of the District of Columbia, an HBCU, which encompassed learning goals related to a variety of disciplines, including social sciences, bioethics, statistics, molecular biology, immunology, and cancer biology, among others. This biology course was a junior-level elective for biology majors, and it focused on both the social and physiological determinants of health disparities. The class was structured as a seminar-style course that included several guest speakers from other institutions lecturing in their areas of expertise. As a guide to develop new courses, institutions can adapt health disparities courses developed for medical education purposes to fit the undergraduate context (Jacobs et al., 2003; Vela et al., 2008; Ross et al., 2010).
Institutions that are unable to develop such a course in their biology department can consider strategies to establish such courses in other departmental units. For instance, science departments can partner with social sciences colleagues at their institutions to develop interdisciplinary courses that integrate the social and biological factors influencing health disparities. Life sciences departments can also take advantage of the growing presence of undergraduate public health programs (Arnold and Schneider, 2010), which might already include health disparities courses or might have faculty with the appropriate expertise to develop such courses. Institutions should consider strategies that advertise courses in various departments to students in scientific majors, in order to make them more visible. These advertising strategies would benefit both institutions that already include health disparities courses in their curriculum and those developing new courses.
Another advantage of health disparities courses is that they can influence how students effectively connect their scientific knowledge with real societal issues. One key competency for undergraduate science students is to understand the relationship between science and society and the implications that scientific discoveries have in that context (American Association for the Advancement of Science [AAAS], 2011). This connection can be effectively implemented through health disparities courses or related activities, because they allow students to associate their scientific foundation with a relevant societal issue. Moreover, the course can also benefit from the rich source of knowledge available from the students themselves, who can contribute their own personal experiences and viewpoints to discussions.
Besides incorporating new courses on health disparities, there are other approaches that can expose students to these issues. University collaborations with the community, state and local governments, and other institutions of higher education, can bring in new opportunities for students to participate in health disparities research or other projects (Carry et al., 2005; Lunn and Sanchez, 2011). For example, undergraduate institutions could partner with local medical schools, which usually are associated with free community clinics with pharmacy, laboratory, and education components, at which undergraduate students could volunteer. Moreover, there have been a number of interventions at the medical school and postbaccalaureate level that could potentially be adapted to and implemented at the undergraduate level. For example, students can be involved in programs with community partners that teach them about underserved populations, they can volunteer their time at a local community clinic, or they can complete community-based participatory research projects around health disparities issues in the area (Jacobs et al., 2003; Ko et al., 2007). Additionally, programs such as the National Institutes of Health (NIH) Academy, a 10-mo training program on health disparities designed for NIH postbaccalaureates, can be used as a model in undergraduate education (NIH, 2014). These types of strategies could be adapted as courses, extracurricular activities, or programs run by an on-campus group or society that is more widely visible among students.
Incorporating health disparities courses and activities into the undergraduate life sciences curriculum can be of additional value in developing the competencies necessary for biomedical professions and in motivating students to help eliminate health disparities during their diverse career paths. As these programs of study are developed, it would be of interest to design discipline-based education research studies to measure the short- and long-term effects of such courses on student motivation, student career choices, and student cultural competency.
ADDRESSING HEALTH DISPARITIES EARLY IN THE EDUCATIONAL PIPELINE
Disparities in health outcomes and healthcare are one of the major current public health concerns. Efforts directed toward eliminating health disparities must be varied and must include training a culturally competent and knowledgeable biomedical workforce. It is crucial to include approaches that target undergraduate education and expose students pursuing biomedical careers to health disparities. Incorporating courses, experience and hands-on activities, and partnerships related to health disparities at undergraduate institutions are approaches that can increase students’ exposure and awareness to these issues. These efforts are particularly important at MSIs, which serve students from communities differentially affected by health disparities who are more likely to work with underserved populations during their careers. The development of a knowledgeable biomedical professional workforce is critical to reduce and eliminate health disparities in highly vulnerable populations.
ACKNOWLEDGMENTS
The authors thank Shifali Arora, Oni Celestin, Sharmi Das, Patricia Forcinito, Natasha Lugo-Escobar, Steve Schultz, and Susan Singer for insightful comments and suggestions. R.B. thanks Beth Mitchneck and Sylvia James for support of this work. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors alone and do not necessarily reflect the views of the National Science Foundation, NIH, AAAS, or any other organizations with which the authors are affiliated. D.K. gratefully acknowledges the support from the CDMPRP Prostate Cancer Research Program (PC073564, PC131862, PC111314) and the National Cancer Institute Center to Reduce Cancer Health Disparities (CA162264).